The Maine Center for Palliative Medicine Nurse Practitioner Fellowship is a one-year program designed to nurture and educate a certified Nurse Practitioner in hospice and palliative care, across a wide range of settings.
Goals of the MCPM Nurse Practitioner Fellowship
MCPM is invested in providing the communities we serve with nurse practitioners with specialty level knowledge in hospice and palliative care.
The NP fellowship program:
- Supports the development of expertise in this field through a comprehensive curriculum, diverse clinical experiences and expert faculty.
- Focuses academically with didactic and project based learning to promote evidenced based practice.
- Embraces partnerships with area institutions to provide additional opportunities for learning and interdisciplinary team work.
Objectives of the MCPM Fellowship
The NP fellow will receive supervision and conditional independence from faculty through didactic and clinical learning in order to achieve successful board certification in Advanced Hospice and Palliative Nursing.
At the end of the fellowship year, the fellow trained nurse will be able to:
- Provide patient centered care that is compassionate, culturally sensitive, appropriate, and effective for the treatment of both common and uncommon health conditions.
- Enhance knowledge of established and evolving biopsychosocial, clinical, epidemiological, and nursing sciences, and use of evidence-based practice.
- Demonstrate the ability to evaluate one’s own practice and improve outcomes with patients. Based on best available evidence, constant self-evaluation and lifelong learning are imperative.
- Facilitate effective communication in collaboration with patients, their families, and inter-professional colleagues.
- Demonstrate commitment to carrying out professional roles and responsibilities while adhering to ethical principles.
- Demonstrate awareness of healthcare systems, fiscal responsibility and the ability to effectively interface with other resources to optimize care.
- Actively participate in providing leadership in health care now and in the future.
- The application period opens on December 1 and can be accessed here.
- Candidates will be reviewed by a selection committee comprised of MCPM nurse practitioners, physicians and Androscoggin nursing leadership
- Interviews will be conducted with qualified candidates
- Timeline:
| Application period opens | December 1, 2023 |
| Application period closes | March 31, 2024 |
| Contacted for interview | April 1, 2024 |
| Fellowship begins | July 1, 2024 |
| Fellowship ends | June 27, 2025 |
Eligibility Criteria
- Completion of accredited nurse practitioner program
- Certification in area of focus which must include care of adult
- Licensure or ability to obtain licensure as a nurse practitioner in the state of Maine
- DEA license for prescribing controlled substances
- Demonstration of clinical excellence through 3 letters of recommendation from clinical preceptors or faculty from NP program, or current colleagues
- Completion of on line application
- Provide curriculum vitae
- Personal statement describing interest in MCPM NP fellowship program, learning objectives for the fellowship year and goals to advance palliative and hospice care in our communities (500 word limit)
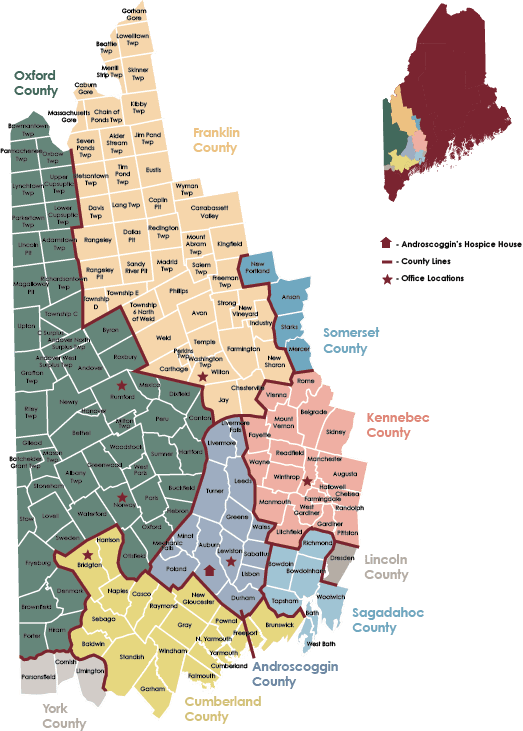
- Ability to participate full time (40 hours per week) in the fellowship program, including travel to multiple sites across MCPM’s service area, and Southern Maine
The curriculum is organized over a 12 month period consisting of clinical, education and scholarly experiences. The program objectives focus on nurturing the NP in the art and science of hospice and palliative care. This is done within a framework of interdisciplinary teams, serving urban and rural communities. This innovative approach to learning focuses on the competencies of evidence based practice and professionalism. The curriculum allows the fellow to participate as a team member at the various clinical sites. The overarching skills of compassion, expert practice and clear communication are the essence of a successful program.
Compensation:
- One year competitive stipend and benefits
- CME opportunities
- Hospice and Palliative Nurse Association membership
- Funding to attend one national conference focused on hospice and palliative care
Clinical rotations will be coordinated by MCPM fellowship directors. Each rotation will be held at the relevant healthcare practice site for at least 1 month. The clinical experiences will expose the NP fellow to varying levels of acuity, diagnoses, and clinical practices. Preceptors at the clinical sites will provide the opportunity to interact with various palliative care interdisciplinary team members at their location. Clinical sites may include:
- Androscoggin Home Hospice Program
- Androscoggin Inpatient Hospice Unit (Hospice House)
- St. Mary’s Regional Medical Center Acute Care
- St. Mary’s Regional Medical Center Oncology Clinic
- MCPM Outpatient Clinic
- Maine Dartmouth Geriatric Clinic
- Maine Medical Center
The curriculum is aligned with National Nurse Practitioner Residency and Fellowship Training Consortium Accreditation Standards and is intended to prepare the learner to transition to an independent role in Hospice and Palliative care. The curriculum builds upon previous NP education and experience. The clinically focused curriculum aims to allow the fellow to meet eligibility requirements to sit for the ACHPN certification exam upon successful completion of the fellowship.
The comprehensive curriculum includes competencies related to knowledge, patient care, evidenced based care, systems based practice, professionalism and communication skills. Learning occurs with educational didactic sessions, mentored clinical experiences, specialty and elective rotations, mentored leadership experiences and professional development activities. Fellows will be expected to produce products of their learning including small group case presentations, quality improvement or research projects and journaling exercises with ongoing self-evaluation.
The program intends to develop an independent nurse practitioner who will:
- Provide patient centered and team based comprehensive, compassionate, culturally sensitive patient and family focused hospice and palliative medical and nursing care with a focus on those communities served by MCPM and fellowship clinical site partners.
- Function as a key professional within the health care team focusing on inclusion, equity, integrity, diversity and respect.
- Develop skills of resiliency and self-care to sustain professional growth and development.
- Transition to a confident and competent independent practitioner utilizing mentorship, didactic lessons, self-directed learning and diverse clinical educational opportunities.
- Develop competencies in communication and as an educator for patients, families and communities.
- Provide disease specific hospice and palliative care including diagnoses, co-morbidities and urgent/emergent complications
Hospice and palliative care patient care
- Provide evidenced based patient centered care that is compassionate, appropriate and effective for health problems.
- Comprehensive Assessment; collect, prioritize and interpret data. Perform a review of systems, physical exam, utilize standardized tools (pain scales, functional assessment).
- Diagnosis and planning. Formulate and prioritize medical and nursing differential diagnosis. Order appropriate diagnostic tests.
- Select appropriate interventions to develop an interdisciplinary plan of care. Perform procedures, prescribe treatments and medications.
- Evaluate outcomes and accurately document care.
- Participate in bereavement support as needed